Treating Patients in Our Preferred Provider Organization (PPO) Plans
Most Peoples Health plans require that members receive care from network providers, except in emergency or urgent situations. Peoples Health offers two PPO plans with out-of-network benefits—Peoples Health Choices (PPO) and Peoples Health Patriot (PPO).
Members of these plans may use their out-of-network benefit to access care from out-of-network providers who are not in the Peoples Health provider network, and higher member cost-sharing may apply. As an out-of-network provider, if you accept Medicare assignment, you may provide care to these members. See our Information for Out-of-Network Providers for details about submitting claims electronically.
Please note: As with all our PPO plans, rendering care to members of a Peoples Health PPO does not mean that you are contracted with Peoples Health.
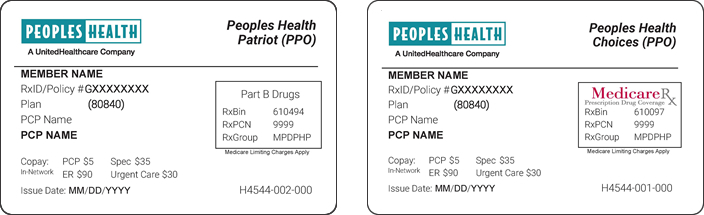
For your reference, below are images of the ID cards for our two PPO plans, which clearly identify the plan as a PPO within the plan name at the top.